What is sciatica?
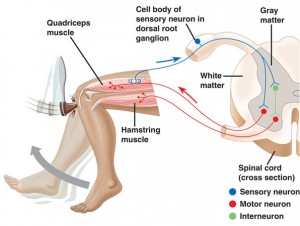
Sciatica is a condition characterized by pain that radiates along the path of the sciatic nerve, which is the longest nerve in your body. The sciatic nerve runs from your lower back, through your hips and buttocks, and down each leg, it provides most of the sensation, muscle strength and reflexes in the leg. Sciatica is not a medical diagnosis in itself but rather a symptom of an underlying condition. Several common causes of sciatica include:
- Herniated or Bulging Disc: The most common cause of sciatica is a herniated or bulging disc in the spine. When the soft inner material of a disc protrudes or leaks out, it can press on the nerve roots that form the sciatic nerve.
- Spinal Stenosis: This is a condition where the spinal canal narrows, putting pressure on the nerves, including the sciatic nerve.
- Degenerative Disc Disease: As the discs in the spine age, they can lose their cushioning ability, leading to pain and irritation of the nerves, including the sciatic nerve.
- Piriformis Syndrome: The piriformis muscle, located in the buttocks, can sometimes irritate or compress the sciatic nerve, causing sciatica.
- Spondylolisthesis: This is a condition where one vertebra slips forward over an adjacent vertebra, putting pressure on the sciatic nerve.
- Pregnancy: In some cases, the pressure of the growing uterus on the sciatic nerve during pregnancy can cause sciatica.
And on rare occasions tumours, infection and injury.

Treatment may involve a combination of pain management, physical therapy, and in some cases, surgical intervention. If you suspect you have sciatica or are experiencing persistent pain, it’s essential to seek professional advice for an accurate diagnosis and appropriate treatment.
Chiropractors use a variety of non-invasive techniques to treat sciatica, with the goal of relieving pain and improving function. It’s important to note that while some people find relief from chiropractic care, however the effectiveness of these treatments can vary. Here are some common chiropractic approaches to treating sciatica:
- Spinal Adjustments (Manipulation): Chiropractors often use spinal adjustments to realign the spine and reduce pressure on the sciatic nerve. This involves the application of controlled force to specific joints, aiming to improve mobility and alleviate pain.
- Flexion-Distraction Technique: This is a gentle, hands-on spinal manipulation technique that involves using a specialized table to stretch and decompress the spine. It can be particularly useful for treating conditions like herniated discs that may be contributing to sciatica.
- Therapeutic Exercises: Chiropractors may recommend specific exercises to strengthen the core muscles and improve the stability of the spine. Strengthening these muscles can help support the lower back and reduce pressure on the sciatic nerve.
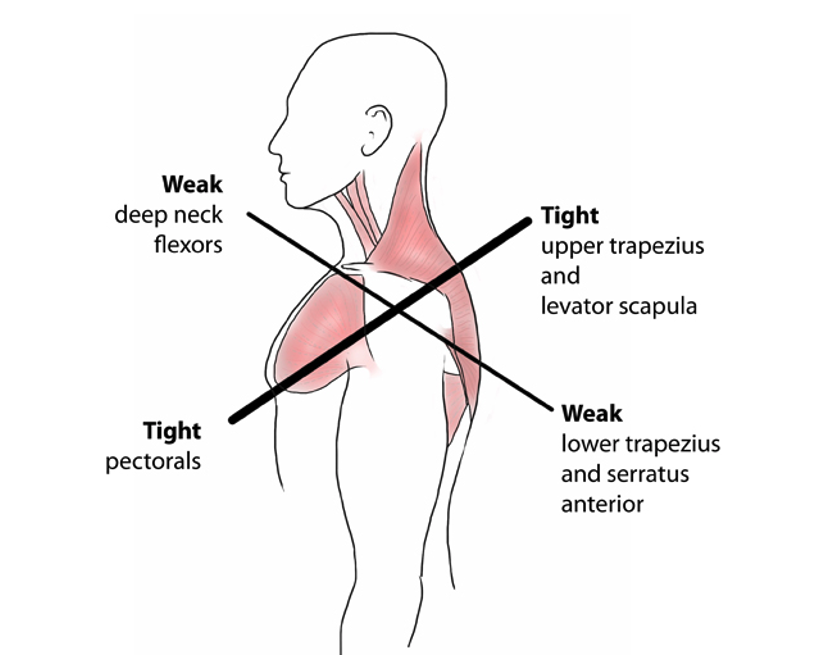
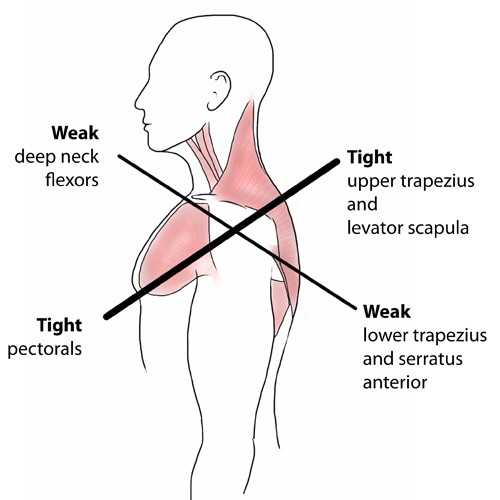
- Lifestyle and Postural Advice: Chiropractors often provide guidance on ergonomics, posture, and lifestyle modifications to help prevent the recurrence of sciatic pain. This may include recommendations for proper sitting, standing, and lifting techniques.

While people experience relief from chiropractic treatments, it is important to acknowledge that others may find more benefit from a combination of approaches, including physical therapy, medication, and, in severe cases surgical intervention is required.
Always discuss your symptoms and treatment options with a healthcare provider, such as chiropractor to determine the most appropriate and evidence-based approach for your specific situation.
Our approach
We have a flexible approach, aiming to find a gentle and effective treatment to suit the needs of you, your lifestyle and your health goals.
Our chiropractor has completed an undergraduate masters qualification in chiropractic, is a member of the British Chiropractic Association (BCA), registered with the General Chiropractic Council (GCC), as well as completing an extra year of pre-registration training to become a member of the College of Chiropractors (CoC).
We take pride in the fact that the majority of our patients come to us through the recommendation of other satisfied patients.